| blog.google |
Welcome to another summer week on The Blog. Yours Truly got a brief scare when she saw that California Governor Gavin Newsom ordered the hair salons and barbershops closed. The good news is it would only be in the counties on the monitor list and for a short period--Blogger hopes. Thank goodness. Really everyone, is that hard to maintain social distance and cover your nose and mouth when you go out? If you want to get back to some version of normal, all you have to do is #WearAMask. Thank you. Onward
Is racism a public health crisis? Yes, says recent article published by The Pew Charitable Trust: "Being black is bad for your health. And pervasive racism is the cause" (pewtrusts.org: June 15, 2020; date accessed July 13, 2020). This is the conclusion the conclusion of multiple public health studies conducted over the past three decades. Dr. George Benjamin, the executive of the American Public Health Association, told the The Pew Trust,
We do know that health inequities at their very core are due to racism,... There's no doubt about that (pewtrusts.org: June 15, 2020).
| publichealthinsider.com |
As a black man, my status, my suit and tie don't protect me (Ibid)
The data tells the grim tale: "Black women are up four times more likely to die of pregnancy related complications than white women. Black men are more than than twice as likely to be killed by police as white men. And the average life expectancy of African Americans is four years lower than the rest of the U.S. population" (pewtrusts.org: June 15, 2020).
These bleak statistics were enough to convince cities and counties in Michigan, Ohio, and Wisconsin to declare racism a public health crisis (Ibid). Supporters believe that the designations are intended to power systemic changes across all sectors of government, such as: criminal justice, education, health care, housing, transportation, budgets, and taxes (Ibid). The ultimate goal is to shrink the chasm in healthcare that separate African and white Americans. Those are the stark facts. The first step in shrinking the chasm is identifying how racist ideas have infiltrated public health then uprooting them.
| pewtrusts.org |
Let us take a step back for a moment and define what is "institutional racism." Institutional racism is a reference "to the ways both state and nonstate institutions discriminate, through policies and practices, on the basis of racialized group membership (ncbi.nlm.nih.gov; Apr. 2018; date accessed July 13, 2020). There are racist arguments that shape the explanations of the healthcare disparities between African and white Americans. "The first argument is the biological inferiority of non-Whites. The second, presently more dominant, hold that defects among Blacks lie not in genetic makeup, but in behavior" (Ibid). Both are are equally heinous theories that have their origins in 18th- and 19th-century medical literature that outlined the inherent inferiority of enslaved people. Shockingly, there was even some question as whether African and White Americans were even part of the same species (Ibid). Essentially, it is the difference between assigning blame because of different genomes and individual behavior.
One example, is the difference in approaches to the opioid epidemic. The astronomic increase in painkiller prescription touched off the current crisis thanks to the pharmaceutical industry's aggressive marketing campaign. The patients who received the medication were depicted as the victims suffering pain from their hardworking lives. The system--i.e. the pharmaceutical companies and medical professionals--as failed, not the people (Ibid). The result was a shift in how opioid addiction was approached; treatment as opposed to incarceration. This sharply contrasted with the perception of African American heroin and crack cocaine addiction is they are criminals. The point here is this "dual narratives--one for Whites that sees poor health driven by difficult life circumstances and one for Blacks that sees personal deficiency--..." (Ibid).
| Douglas County, Nebraska Health Department infographic wowt.com |
| newswire.com |
A recent article in the British medical journal Lancet declared,
Racism is a public health emergency of global concern,... It is the root cause of continued disparities in death and disease between Black and white people in the USA. (washingtonpost.com; July 11, 2020; date accessed July 13, 2020)
An editorial in the New England Journal of Medicine summed up the matter,
Slavery has produced a legacy of racism, injustice, and brutality that runs from 1619 to the present, and that legacy infects medicine as it does all social institutions. (Ibid)
Since the beginning of the pandemic, African Americans have been going down and dying from the virus at higher rates than Whites. The NEJM editorial noted further,
...when physicians describing its manifestations have presented images of dermatologic effects, black skin has not been included. The 'covid toes' have all been pink and white. (washingtonpost.com; July 11, 2020)
African Americans also die younger than their white counterparts and have higher rates of death from a string diseases including heart disease, diabetes, cancer, stroke, and asthma (washingtonpost.com; July 11, 2020).
 |
| publichealthpost.org |
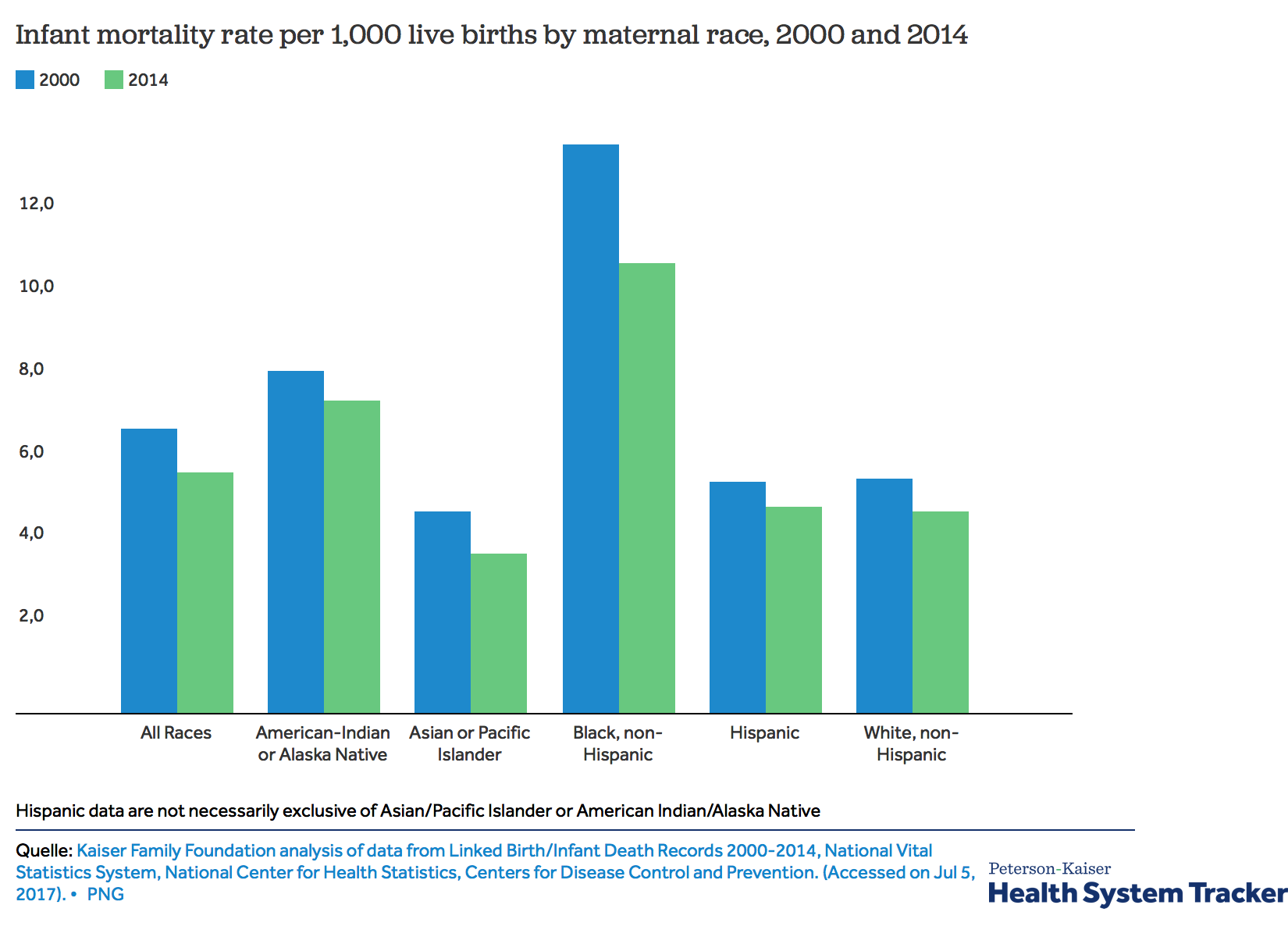
By one measure, African Americans are worse off than they were during slavery. The infant mortality rate--defined as infants who die before their first birthday---is twice the rate than White infants. Specifically: "11.4 deaths per 1,000 live births for blacks compared with 4.9 for whites. Historians estimate that in 1850 it was 1.6 times higher for blacks--340 per 1,000 vs. 217 for whites." (washingtonpost.com; July 11, 2020)
Natalie DiCenzo, an OB/GYN who is about to begin her practice in New Jersey this fall, told The Washington Post, that she hopes to find a way to close the infant mortality gap. "Awareness of racism is necessary for change,..." (Ibid). Dr, DiCenzo said,
I realize that fighting for health equity is often in opposition to what is valued in medicine,...As a white physician treating black patients with a racist health-care system, where only 5 percent of physicians identify as black, I recognize that I have benefited from white privilege, and I now benefit from the power inherent to the white coat. It is my responsibility to do the continuous work of dismantling both, and to check myself daily. (washingtonpost.com; July 11, 2020)
As for covid-19, the Centers for Disease Control say "although black people are dying at a rate of 92.3 per 100,000, patients admitted to the hospital were most likely to be white, and they die at a rate of 45.2 per 100,000." (washingtonpost.com; July 11, 2020) The CDC say, "...racial discrimination puts blacks at risk for a number of reasons, including historic practices such as redlining that segregate them in densely populated areas, where they often must travel to get food or visit a doctor." (washingtonpost.com; July 11, 2020) Specifically,
For many people in racial and ethnic minority groups, living conditions may contribute to underlying health conditions and make it difficult to follow steps to prevent getting sick with COVID-19 or to seek treatment if they do get sick... (washingtonpost.com; July 11, 2020)
The CDC recommends all healthcare providers to follow a standard protocol with all patients and to
[i]dentify and address implicit bias that could hinder patient-provider interactions and communications. (washingtonpost.com; July 11, 2020)
The healthcare system is only as good as the people who work it. The men and women who enter the healthcare professions come with their own ingrained biases that are a product of their education and cultural background. They are not necessarily bad people who deliberately undermine the care of their patients, just people who need to be made aware of the fact that their implicit biases are harming their patients. More than that, we to look at the institutions that impact everyone's health and well-being, and advocate for changes. This is the hard part because public policy changes, for the better, do not happen over night. Hopefully with the attention focused on racial justice, those changes will happen, if we, as a society, make it so.
No comments:
Post a Comment